1. How can Relactagel help?
Relactagel rapidly, effectively and safely treats and prevents Bacterial Vaginosis (BV) through the regulation of vaginal pH. By regulating the vaginal pH, Relactagel neutralises embarrassing odour, relieves abnormal discharge and vaginal discomfort. The lactic acid in Relactagel restores and maintains the natural acidity of the vagina thereby creating a suitable environment for lactobacilli to re-establish. The glycogen content of Relactagel supplements vaginal glycogen and provides nutrients for these naturally occurring lactobacilli. As well as relieving the symptoms of Bacterial Vaginosis, Relactagel can be used to maintain the natural pH balance of the vagina, thereby preventing a recurrence of BV in the long term.
Relactagel is a natural approach to the management of Bacterial Vaginosis through the regulation of vaginal pH.
Relactagel contains no preservatives and can be used during pregnancy.
2. How Relactagel can help your patients?
Over a period of 20 years lactic acid gel has been clinically proven to be safe and highly effective in treatment and prevention of Bacterial Vaginosis. Relactagel has proven efficacy both on its own and in combination with antibiotics to manage the incidence and recurrence of BV. Containing both lactic acid and glycogen, Relactagel helps re-establish the vaginal microbial environment by: lowering the vaginal pH to physiological levels, thereby encouraging the growth and proliferation of vaginal lactobacilli.
3. What is BV?
Bacterial Vaginosis (BV) is the most common cause of abnormal discharge in women of childbearing age. BV is caused by an imbalance in the naturally occurring microbial flora where the predominant lactic acid producing Lactobacillus species are replaced by pathogenic bacteria. BV should not be confused with a yeast infection (Candidiasis), or an infection with the parasite Trichomonas vaginalis (Trichomoniasis) BV is not generally considered to be a sexually transmitted infection.
A healthy vagina normally contains many microorganisms primarily Lactobacillus species such as Lactobacillus crispatus and Lactobacillus jensenii. Lactobacillus (LB) are a genus of commensal (benign) bacteria that colonise the mucosal surface of the vagina. Vaginal glycogen is broken down by human alpha-amylase and then converted into lactic acid by lactobacilli, creating an acidic environment in which they thrive. Lactobacilli form a crucial component of the innate immune system and are found in the vagina and GI tract where they inhibit the growth of pathogenic species of bacteria by:
- Competing for fermentation substrates
- Lowering pH through production of lactic acid
- Production of natural bactericides e.g. cytolysins
Lactobacilli are highly sensitive to changes in their natural environment often brought about by physiological and external factors such as: falling oestrogen levels; antibiotic therapy; exposure to detergents; smoking; stress; sexual activity and the use of IUDs. This altered environment can lead to an overgrowth of pathogenic species of bacteria such as Gardnerella vaginalis, Mobiluncus, Bacteroides, and Mycoplasma. These bacteria are often found at low levels in the vagina however, given an opportunity to proliferate they do so. Upon reaching significant numbers BV associated bacteria begin to produce toxins that interfere with the mucosal immune system, and break down the protective mucus layer leading to a characteristic discharge.

4. Signs and Symptoms
The most common symptom is a thin homogeneous white or grey malodorous discharge which is characteristic of BV. On examination, this discharge is observed to coat the walls of the vagina. Most women with BV do not usually complain of vaginal irritation or discomfort. Often women present with no symptoms, however BV may be diagnosed when vaginal swabs are taken for other indications. In contrast, a ‘normal’ discharge is odourless and will vary in consistency and amount with the menstrual cycle.
5. Diagnosis of Bacterial Vaginosis
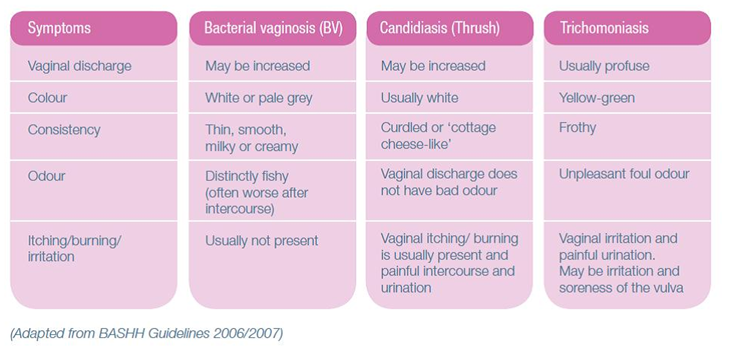
A healthcare professional seeing a woman present with vaginal discharge may consider the following conditions:
- Is discharge normal for this patient?
- Could it be Candidiasis (Thrush)?
- Could it be Trichomoniasis, an infection caused by Trichomonas vaginalis?
- Bacterial Vaginosis
Simple tests can be done to make a proper diagnosis. During a speculum examination some swabs should be taken from high in the vagina to confirm bacterial vaginosis. Under certain circumstances a diagnosis of BV can be made and treatment initiated without further investigations on the basis of:
- A history of recurring BV
- Symptoms and signs including an assessment of the discharge (Table 1)
- Measuring the pH of the vaginal fluid using pH paper (pH > 4.5 indicative of BV)
6. Investigations
When women of reproductive age present with vaginal discharge the following algorithm can be used to identify the most appropriate treatment.

The ‘gold standard’ criteria for diagnosis are based on Amsel’s criteria. An alternative is to use a Gram-stained vaginal smear, with the Hay/Ison criteria or the Nugent score (below). However these are not always practical in primary care.
7. Antibiotic use and Relactagel
Antibiotics in the form of metronidazole or clindamycin are conventionally prescribed to treat bacterial vaginosis. However, the recurrence rate of BV with antibiotics therapy can be as high as 58% 12 months post treatment1. Relactagel has been shown to be proven and effective alternative to antibiotics for the treatment and prevention of Bacterial Vaginosis.
Relactagel has been shown to be effective as oral metronidazole, 500mg twice daily for 7 days and that further intermittent treatment with Relactagel reduces symptoms of bacterial vaginosis and promoted the re-establishment of normal vaginal lactobacilli flora 2,3.
Not only is Relactagel shown to be as safe and as efficacious as metronidazole in the treatment of BV but there is further evidence that when combined with metronidazole is superior to metronidazole alone in promoting lactobacilli colonization5. It has been claimed that maintaining the vaginal pH at or below 4.5 during antibiotic treatment is the most successful approach5.
Due to the combined-action of restoring and maintain the vaginal pH at 4.5, Relactagel not only inhibit the overgrowth of pathogens, but lactic acid content regulates the natural acidic environment so that lactobacilli can become re-established and glycogen content acts as a nutrient to further support lactobacilli. Lactic Acid gel has been shown to be safe and effective in the treatment of BV during pregnancy4.

Depending on whether you are advising the product to treat symptoms, or prevent symptoms from occurring or recurring, Relactagel should be used in different amounts and for differing lengths of time.
For treatment: Use 1 single tube daily for 7 days at bedtime.
For prevention: Use 1 single tube daily for 2-3 days at bedtime after menstruation.
- Bradshaw CS, Morton AN, Hocking J, Garlan SM, Morris MB, Moss LM, Horvath LB, Kuzevska I and Fairley CK. (2006) High recurrence rates of bacterial vaginosis over the course of 12 months after oral metronidazole therapy and factors associated with recurrence. Journal of Infectious Disease, 193 (11), 1478-1486.
- Andersch B, Lindell D, Dahlén I and Brandberg A. (1990) Bacterial vaginosis and the effect of intermittent prophylactic treatment with an acid lactate gel. Gynecologic and Obstetric Investigation, 30(2), 114-119. Erratum in: (1991) Gynecologic and Obstetric Investigation, 31(1), 7.
- Andersch et al (1986) Treatment of bacterial vaginosis with an acid cream: a comparison between the effect of lactate-gel and metronidazole. Gynecol Obstet Invest. 21: 19-25.
- Holst and Brandberg (1990) Treatment of bacterial vaginosis in pregnancy with lactate gel. Scand J Infect Dis. 22: 626-626
- Decena et al (2006) Metronidazole with Lactacyd vaginal gel in bacterial vaginosis. Obstet Gynaecol Res. Vol 32, 2: 243- 251.
8. How does Relactagel work?
Relactagel contains lactic acid which helps to restore the normal acidic pH balance of the vagina. It also contains glycogen which provides nutrients to lactic acid bacteria. When the normal pH balance and nutrients are present in the vagina this enables lactic acid bacteria to grow and restores the natural balance of vaginal flora.
The recommended Relactagel dosage is as follows:
For treatment: Use 1 single tube daily for 7 days at bedtime.
For prevention: Use 1 single tube daily for 2-3 days at bedtime after menstruation.
9. How to use Relactagel?
Relactagel is a fast, effective and safe way of treating and preventing Bacterial Vaginosis. The recommended Relactagel dosage is as follows:
For treatment: Use 1 single tube daily for 7 days at bedtime.
For prevention: Use 1 single tube daily for 2-3 days at bedtime after menstruation.
Step 1: Relactagel comes in a pack of 7 single-use applicators. To use Relactagel, simply break and remove the cap on the applicator.
Step 2: Insert the entire neck of the applicator into the vagina. Relactagel should be used at bedtime when lying down to minimise any potential leakage.
Step 3: Squeeze out the contents of the applicator, maintaining constant pressure while withdrawing the applicator.
In the event of leakage, a panty liner may be useful. Once opened use immediately.
Warning:
Relactagel may cause mild irritation during fungal infections (e.g. thrush) of the vagina or when there are tears in the vaginal tissue.
Relactagel contains glycogen obtained from Oysters. Do not use if allergic to shellfish.
10. Clinical Evidence Supporting Lactic Acid Gel
There is a wide body of clinical evidence supporting the use of Relactagel. Please see below links to clinical papers looking at the use of lactic acid gels for the treatment and prevent of Bacterial Vaginosis.
Efficacy
In a study by Decena et al (2006) lactic acid was shown to be as effective as metronidazole in the treatment of BV. Lactic acid gel is well-tolerated and suitable for use during pregnancy (Holst 1990) and it is less likely to result in the characteristic recurrent foul smelling discharge associated with BV when compared to metronidazole alone (6.7% v 14.3%). (Decena,2006)
Decena et al (2006) Metronidazole with Lactacyd vaginal gel in bacterial vaginosis. Obstet Gynaecol Res. Vol 32, 2: 243- 251.
Holst and Brandberg (1990) Treatment of bacterial vaginosis in pregnancy with lactate gel. Scand J Infect Dis. 22: 626-626
Recurrence
In their overview of BV treatments Larsson and Forsum (2005) stated that long-term follow-up after treatment (longer than 4 weeks) shows a relapse rate of 70%. Interestingly, Larsson concluded in this paper that there is little difference in recurrence rates manifested between available treatments.
Furthermore, Bradshaw et al (2006) showed ‘high recurrence rates of BV (58%) … over the course of 12 months in women treated for 7 days with oral metronidazole’.
Larsson PG and Forsum U. (2005) Bacterial vaginosis-a disturbed bacterial flora and treatment enigma. APMIS, 113, 305-316.
Bradshaw CS, Morton AN, Hocking J, Garland SM, Morris MB, Moss LM, Horvath LB, Kuzevska I and Fairley CK. (2006) High recurrence rates of bacterial vaginosis over the course of 12 months after oral metronidazole therapy and factors associated with recurrence. Journal of Infectious Diseases, 193(11), 1478-1486.
Prophylactic Treatment
Lactic acid gel was used prophylactically in a double blind trial conducted by Andersch et al (1990) and it was found that for those patients treated with lactic acid gel for 6 months, 88% showed no sign of BV in comparison to the placebo group in which the response was substantially poorer with only 10% showing no signs of BV (p<0.001).
Andersch B, Lindell D, Dahlén I and Brandberg A. (1990) Bacterial vaginosis and the effect of intermittent prophylactic treatment with an acid lactate gel. Gynecologic and Obstetric Investigation, 30(2), 114-119. Erratum in: (1991) Gynecologic and Obstetric Investigation, 31(1),7.
Combination Treatment
A further finding in the Decena et al (2006) study was that lactic acid gel, when combined with oral metronidazole, is ‘superior’ to oral metronidazole alone in promoting lactobacilli colonisation. The authors found that using lactic acid gel in combination with metronidazole resulted in the lowest number of recurrent BV episodes. Similar conclusions were made by Wilson (2004) who stated: ‘… it appears that a rise in vaginal pH allowing the overgrowth of bacteria may be more important than reduction of lactobacilli. However, long term colonisation with lactobacilli is necessary to help maintain an acidic pH… Therapies aimed at one aspect of this inter-relation may help some women with recurrent BV, but a combined approach might work better. Probably the ideal way of managing recurrent BV would be to tackle all aspects of the inter-relation by replacing the lactobacilli, at the same time maintaining the vaginal pH at 4.5, and if necessary also adding in prophylactic treatment to control overgrowth of bacteria’.
Decena et al (2006) Metronidazole with Lactacyd vaginal gel in bacterial vaginosis. Obstet Gynaecol Res. Vol 32, 2: 243- 251.
Wilson, J. (2004) Managing recurrent bacterial vaginosis. Sexually Transmitted Infections, 80, 8-11.
Non-invasive/non-antibiotic treatment
It was shown that the treatment of BV with a lactic acid gel in ten pregnant women resulted in renewal of the normal vaginal flora 8 weeks after completion of treatment, 8/10 women were cured ie. Did not fulfil any of the 4 clinical criteria for BV and had a normal lactobacillus flora. Therefore this approach is an alternative to antibiotic treatment for patients with recurrent BV especially during pregnancy (Holst et al, 1990).
Holst and Brandberg (1990) Treatment of bacterial vaginosis in pregnancy with lactate gel. Scand J Infect Dis. 22: 626
11. Relactagel Availability
Relactagel® is available both over the counter from your local pharmacy and can also be purchased online/
All online purchases can be sent to a delivery address of choice and is shipped in discreet packaging.
Downloads for HCPs
Download Healthcare Professional Brochure
Download Healthcare Professional Data Sheet
